D epression is a dysregulation of the brain function that control emotions (or moods). It is a mood disorder characterized by intense and persistent negative emotions. These emotions negatively impact people’s lives, causing social, educational, personal and family difficulties.
Depression is different than feeling sad or down. It is a medical condition affecting the way mood is controlled by the brain. Someone with Depression can’t just “snap out of it.” Depression affects the way a person thinks, feels and acts. It becomes a negative lens through which they see and experiences the world.
When Depression happens, it often lasts for many months and then sometimes gets better. This is called an episode of Depression. Most people who get Depression will experience many episodes during their lifetime. Depression is often called Major Depressive Disorder (MDD).
Sometimes a negative event (such as the loss of a loved one, or severe and prolonged stress) will trigger an episode of Depression but often episodes will occur spontaneously. Depression is not caused by the usual stresses of life. Depression is often accompanied by feelings of anxiety and causes significant problems with family, friends, work or school.
In a one-year period, approximately 7 percent of people will experience Depression. It is most common in women and in young adults, and the first episode often begins in the teen years or early adulthood.
Depression is the result of dysregulation in the brain circuits that control emotional functioning. It is not related to someone’s ethnic background, level of education, how much money they make, or their relationship status. We do know that Depression runs in families, so people with immediate family members (e.g., parent, sibling, or child) with Depression are more likely to develop Depression themselves. Beyond this genetic component, some people develop Depression following a major stressor (e.g., relationship breakup, job loss) or significant trauma (e.g., death of a loved one, abuse, or neglect; especially as a child). Research has found that the impact of stressors may depend on your genetics, as some people’s genetics make them more vulnerable to stress than others. There are also certain medical conditions and medications that can sometimes lead to Depression.
Depression, and other mental disorders, should only be diagnosed by a medical doctor, clinical psychologist, or a trained health provider who has spent time with the person and has conducted a proper mental health assessment. Diagnoses are complicated with many nuances. Please do not attempt to diagnose someone based on the symptoms you read about in magazines or on the internet. If you are concerned, speak to a trained health professional.
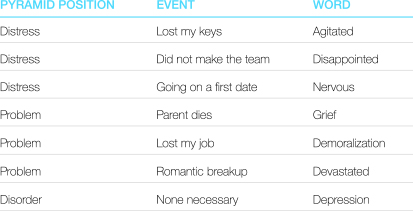
It can be confusing when people use the word “depression” to mean different things. We should try to save the word “depression” to mean the mental disorder of Depression, and use other, more exact words to describe the negative emotions that we feel.
Use the Right Words!
There are 3 types of depressive disorders:
Major Depressive Disorder (MDD)
Someone with MDD will experience episodes of intense depression (lasting weeks to years), separated by periods of relatively stable mood. When people refer to Depression, they usually mean MDD.
Persistent Depressive Disorder (formerly Dysthymia)
People with Persistent Depressive Disorder will experience depressive episodes that are less intense than in MDD but last much longer. For teenagers, these depressive episodes last at least one year and for adults, they last two years or more.
Disruptive Mood Dysregulation Disorder
Children up to 18-years-old can be diagnosed with Disruptive Mood Dysregulation Disorder if they have persistent irritability and frequent episodes of unreasonable verbal and physical aggression.
To determine if someone you care about may be at risk for Depression, consider the following questions:
- Does the person feel sad or low most of the time?
- Has the person lost interest in activities they usually enjoy?
- Do they have trouble concentrating?
- Do they feel fatigued or tired much of the time?
- Do they feel hopeless or worthless?
- Do they experience much less enjoyment in life?
- Has this behaviour lasted at least two weeks, and been present every day for most of the day?
There are three areas of symptoms that often present in youth experiencing depressive episodes. Here are some things to watch for:
Mood
- Feeling persistently depressed, sad, unhappy or something similar
- Feeling a loss of pleasure, or a noticeable disinterest in all or almost all activities
- Feelings of worthlessness, hopelessness or excessive and inappropriate guilt
Thinking
- Diminished ability to think, concentrate or make decisions
- Suicidal thoughts/plans or preoccupation with death and dying
Body Sensations
- Excessive fatigue or loss of energy
- Significant sleep problems (difficulty falling asleep or sleeping excessively)
- Physical slowness or, in some cases, restlessness
- Significant decrease or increase in appetite that may lead to noticeable weight change
If someone in your life has five of the above symptoms (with at least one of them being a mood symptom) present every day for most of the day during the same two week period, then they may be experiencing Clinical Depression (MDD). Talk to your family doctor about your concerns. This behaviour cannot be due to a substance, medicine or another illness and must be different than the individual’s usual mood state.
*In accordance with the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition.
Remembers, you cannot diagnose someone with Depression without a proper mental health assessment conducted by a properly trained health provider.
Consider talking to the person, asking how they are feeling. For example:
- I notice you don’t seem to be as excited about soccer anymore. You used to love it. Has something changed? Have you lost interest in it?
- I’ve been noticing that you’re not yourself lately. How are you feeling?
Early identification and effective intervention is the key to successfully treating Depression and preventing future problems. You can help someone who may be experiencing Depression by arranging or encouraging a meeting with a qualified health practitioner to ensure a proper mental health assessment is done. You can do this in a respectful and nonjudgmental manner.
If someone in your life has been diagnosed with Depression, here’s what you can do:
- Be well-informed. Learn everything you can about Depression and how it may affect the life of the person you care about. Read books, trusted websites and talk to your doctor. Check out Evidence Based Medicine for information on how to critically evaluate the information you read and Communicating With Your Health Care Provider for a list of questions to ask your health care provider.
- Help them get professional help. If it is your child who has Depression, find out from the health provider how you can best help. If it is your friend who has Depression, be there to support them.
- Try not to take any rejection of your efforts to help personally. Remember that Depression causes people to perceive things as more negative than they actually are. Don’t give up but also don’t persist with things that are not helpful!
- Even when it’s challenging, remember that the person needs to know that you care about them. Depression can make it difficult for them to reciprocate or acknowledge your caring but it’s so important to show them that you care.
- Reassure the person that with proper treatment, they will be able to have a positive future and live a healthy and productive life.
- Encourage and help the person maintain a healthy lifestyle. This includes regular physical exercise, enough sleep, and healthy eating habits. For information on healthy sleeping habits, check out Healthy Sleeping.
- Listen. When you listen to and acknowledge someone’s feelings, it sends the message that you care. Knowing that you have people who care about you is an important part of coping with any mental disorder.
- Be patient. Sometimes it can be frustrating when the person you care about doesn’t want to do the things that they used to. Take a deep breath and remember that Depression is making them feel this way. They can’t just “snap out of it.” Getting impatient will only make the situation worse. Stay positive and be patient.
Treatment is used to decrease the length and severity of depressive episodes and prevent new episodes from happening. Successful treatment of Depression leads to much better outcomes in all areas of life and decreases risk of suicide. A variety of treatment options exist for Depression. Determining which course of action is appropriate for each individual should be done with the guidance of a trained health professional. Some options include:
- Psychological Treatments: Psychological treatments or “talk therapy” works by helping your brain better control your thoughts and emotions. There are two different types of psychotherapy that have been found to be effective for treating Depression – Cognitive Behavior Therapy (CBT) and Interpersonal Therapy (IPT). These therapies can be done one-on-one with a therapist or in a group, and may have a family component (to help parents and siblings understand Depression and learn how they can help).
- Medication: Medication helps the brain correct the functioning of its emotional control circuits. The most common medication prescribed for Depression is a type of antidepressant called Serotonin Specific Reuptake Inhibitors (SSRIs). For more information on how to properly use medications, check out MedEd.
- School Supports: Sometimes certain adaptations can be made by the school to assist a student in coping with and managing their symptoms.
- Community Supports: Community supports can include peer support groups, support groups for families, and other helpful resources.
- Regular Routine: Maintaining a healthy, regular daily routine is very important for a person with Depression. For help maintaining the kind of healthy lifestyle that should accompany professional treatment for Depression, check out Taking Charge of Your Health.
Most often, people with Depression will be treated with both medication and psychotherapy – medication for short-term improvement and psychotherapy for long-term change. Some people may need to have both medication and psychotherapy for a substantial period of time to keep well.
People with Depression are at increased risk for suicide, especially if the Depression is left untreated. Pay attention to the person’s behaviour and be aware of the warning signs that they may be contemplating suicide:
- Intense hopelessness or sadness
- Preoccupation with death
- Loss of interest in regular activities
- Withdrawal from family and friends
- Talking about what it will be like when they are gone
- Giving away valued possessions
If you suspect that someone close to you is thinking about suicide, ask them about it and let them know you are concerned. Asking about suicide will not put the idea in their head. Suicidal thoughts must be taken seriously and should never be ignored. Take the person to the hospital immediately or call 911. Suicide risk is serious and there are professionals who can help. Click here for more information on youth suicide.
It’s not uncommon for people to have more than one mental illness. Other common co-occurring disorders with Depression (also called comorbid disorders) include:
- Anxiety Disorders (such as Social Anxiety Disorder or Panic Disorder)
- Obsessive-Compulsive Disorder
- Alcohol or Drug Use Disorders (Substance Use Disorders)
- Eating Disorders
- Suicide
- TeenMentalHealth Speaks… Depression
- Could My Parent Have Depression?
- Communicating with your Health Care Provider
- Healthy Sleeping
- Evidence Based Medicine for Patients and Youth
- Could My Sibling Have a Mental Illness?
- Transitions
- Teening Your Parent
- Parenting Your Teen
- Teen Brain
- Teen Behaviour